MEDICARE PART D SECTION 3
TRACKING THE COVERAGE GAP
Carriers will send out statements when their members purchase prescription drugs to show them the costs, how close they are to the coverage gap, and if the member is in the coverage gap, how much further they need to go until they reach catastrophic (post coverage gap) coverage.
FORMULARIES
Formularies are the list of covered drugs each plan has. Each carrier has the ability to choose what drugs they will cover and place in them in the tier level of their choosing.
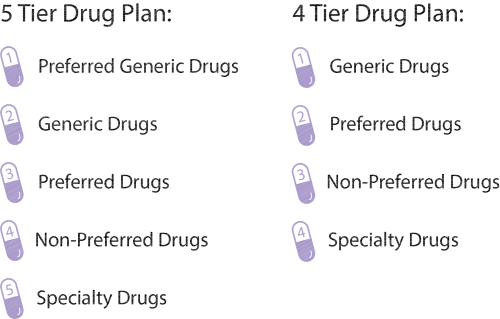
Most plans have a 4 or 5 tier level system:
It is important to make sure the drugs they are currently on match the tier levels or your clients are aware of the different tiers so there are no drastic cost differences.
NETWORK VS PREFERRED PHARMACIES
Network pharmacies are pharmacy locations members can use
Preferred are in-network pharmacies which have special negotiated prices to help lower member drug costs
Mail order is also a common option. Many larger Part D carriers own their own mail order service and offer even greater savings to their members
PART D PENALTY
For each month a Medicare beneficiary is eligible for a Medicare Part D plan and does not have one or any other credible coverage, they will be have to pay 1% of the national average for each month they were eligible.
The penalty will be assessed by the Social Security office and will stay with the beneficiary for life.
FLASHCARDS! HOVER OVER EACH CARD
TO SEE THE CORRECT ANSWER
